What is a normal pregnancy?
It is a pregnancy which is not associated with any medical/surgical condition in the pregnant lady or her fetus, ending in delivery of a single, healthy, mature neonate at full term.
What is the duration of a normal pregnancy?
Most of the general population calculate gestational age and date of delivery based on calendar months. Actually, this creates daily misunderstanding between obstetricians and pregnant women, since most ladies calculate a pregnancy starting their ovulation or missed period dates. They do not take into consideration the differences in the number of days between different months which eventually creates more difference in the calculated gestational age. This is why it is always best to calculate such dates by weeks starting on the first day of the last period (on the condition that this last period was a normal and regular one) since this date is usually easily identified in most women. So, a normal pregnancy should last for 40 weeks (roughly 9.3 months), including the first ±2 weeks of the cycle causing the pregnancy.

What are the stages of a normal pregnancy?
The first stage is that of organ appearance (organogenesis), lasting till 10 weeks gestational age. This is the period where most congenital malformations develop should the pregnant lady get exposed to different risk factors, such as infections, chemicals or medicines, radiation and some risky medical condition (e.g. uncontrolled diabetes mellitus). This is why it is always advisable to consult your obstetrician before planning a pregnancy, since the first 4-5 weeks usually pass before the lady knows that she is actually pregnant, missing a considerable part of the duration of fetal organogenesis.
Then come the weeks 10 to 14, where risks of miscarriage start dropping considerably, especially following ruling out congenital malformations using blood tests and ultrasonography.
The following 14 weeks (thus reaching a gestational age of 28 weeks) are the phase of fetal growing. Yet, this is not the phase of fetal maturity; so a delivery at such dates is called a late miscarriage or a very preterm delivery. This period, in most healthy women, passes uneventfully, having passed the stage of nausea and fatigue of early pregnancy and having a baby that is not yet big enough to limit the woman’s activity. The most important events during this stage are the ultrasound anomaly scan at around 20 weeks, the transvaginal scan for estimation of cervical length (and hence the risks for preterm delivery) and the blood screening test for diabetes mellitus.
The weeks 28 to 37 represent the stage of accelerated fetal growth as well as the gradual maturation of organ function. Therefore, each day that passes makes a difference in the neonatal ability to survive after birth. The risks of needing neonatal admission to special care units drop as pregnancy advances. Furthermore, this is the period where follow up of blood pressure as well as fetal growth becomes most crucial. Premature labor pains before full term would usually need intervention to try to stop the womb from going into active labor by giving medicines t stop uterine contractions (tocolytics) to give the fetus a chance to mature a little more before it is born.
Last comes the 37 to 40 weeks, where >90% of deliveries should happen. A lady who does not go into spontaneous labor within 10 days after full term would usually need medical induction of labor.
And what are the normal changes or symptoms which happen during pregnancy?
Most women experience some nausea or mild vomiting during the first trimester of pregnancy which are more common in the morning or following heavy meals. Ladies may feel tired and sleepy, with some difficulty to concentrate for long periods of time. They usually complain of constipation and frequency in micturition.
During the 14th – 28th weeks, the growing size of the pregnancy causes some discomfort in the two sides of the abdomen which increases during movement. It is also not uncommon to feel few uterine cramps in the midline of the abdomen, especially just above the bikini line, but these cramps should be few, not associated with pain and not leading to changes in the measurements of the neck of the womb (the uterine cervix) on ultrasonography. This stage is also frequently associated with low blood pressure and feeling faint. The woman usually can perceive fetal kicks starting around 20-22 weeks. These may not become regular till 26-28 weeks, most babies move more at night.
The period between 28 to 37 weeks is the most crucial period during pregnancy. Babies start having a fair chance of survival if delivered prematurely for any reason, which of course increases as pregnancy advances. Most pregnancy complications (such as hypertension, diabetes mellitus, and slow fetal growth) get more likely as pregnancy advances, while most babies are still not mature enough. This may put the doctor in face of a difficult decision to make: whether to deliver the lady for her own sake or to carry on the pregnancy for a little longer for the sake of the neonate. This period is also associated with progressive difficulty in movement, a feeling of fatigue, indigestion and heartburn. The symptoms of anemia, vitamin or calcium deficiency may start to present. Hence, a good doctor should be able to identify risk factors early enough to avoid or at least reduce their harms.
 Finally, during the period between 37 weeks and full term, the fetus would have functionally matured but would continue to grow still. Labor pains may start any point in this period, but it is generally advisable not to electively deliver the woman before the completed 39th week to further reduce the risks of neonatal complications. The doctor can predict (through pelvic clinical and ultrasonographic examination) any problems which may prevent normal delivery, so as to put the best and safest plan for an easy and successful delivery.
Finally, during the period between 37 weeks and full term, the fetus would have functionally matured but would continue to grow still. Labor pains may start any point in this period, but it is generally advisable not to electively deliver the woman before the completed 39th week to further reduce the risks of neonatal complications. The doctor can predict (through pelvic clinical and ultrasonographic examination) any problems which may prevent normal delivery, so as to put the best and safest plan for an easy and successful delivery.
What is the nutritional plan during pregnancy?
The fetus needs extra amounts of calories and a balance diet from the mother for successful development throughout pregnancy. The normal weight gain during pregnancy is 12-15 Kg, most of which occurs in the second half of pregnancy. After delivery, your bodyweight goes back to normal gradually over the first 6 months, except for 5-7 Kg which would need diet and physical exercise to be lost. Generally, strict or hard diet to lose weight is not advisable during pregnancy or in the first few months after delivery since this may harm the growth and development of your baby.
As for your diet, the average pregnant woman needs 30 Kcal. / Kg prepregnacy body weight, together with 1.5 Litres of water. It is advisable to divide your meals into frequent small portions to avoid indigestion, heartburn or constipation. It is also advisable to have plenty of proteins (meat, fish, poultry, milk), a moderate amount of fibres (in the form of fruits and green vegetables as well as bread), and small amounts of fats (such as full cream milk, white cheese). It is best to avoid large amounts of simple sugars, salt, caffeine and chocolates.
The pregnant lady should try to include a weekly course of fish to supply the baby with enough iodine lady necessary for brain development. She should make sure she eats enough fresh fruits or vegetables and salads containing vitamins (since the latter may be destroyed by cooking). Direct exposure to sunlight is crucial for building enough stores of vitamin D.
The pregnant should keep in mind to wash her hands, cooking utensils and fresh food very well before eating to avoid infections which may harm the baby. This is not just to avoid gastrointestinal infections (causing diarrhea or stomach aches), but to avoid some infections which may be transmitted by oral routes following exposure to dust or flies and may cause serious birth defects. Also, it is advisable to avoid canned or delivery food as well as undercooked cheese, meat or seafood.
What about multivitamins and mineral supplements during pregnancy?
It is best to consult your doctor first, since some of these supplements may contain doses which are ineffective or, more importantly, harmful to the pregnancy. Generally, we advise using folic acid supplements at least during the first trimester, since it was proven that this vitamin prevents some types of serious birth defects. Most healthy women would not need other vitamin supplements except in case of iron, calcium or vitamin D deficiency.

What about medications and vaccinations during pregnancy?
We generally advise avoiding medicines during the first trimester. But when needed, some types of medicines are safer than others during pregnancy (consult your doctor about all medicines before starting them).
As for vaccinations, the allowed types are the microbe-killed types, such as influenza, hepatitis B and tetanus vaccines. While the live-attenuated types are contraindicated during or immediately before pregnancy (such as german measles or chickenpox).
Is it safe to exercise or travel during pregnancy?
Of course it is! But within reasonable limits. Walking and swimming are advisable, but the pregnant woman should wear comfortable sports wear to avoid excessive sweating or heat strokes. She should try to avoid high heels which may cause back and knee pains.
As for travelling, this is allowed provided you avoid prolonged sitting for over 2 hours continuously. You should also drink extra amounts of fluids and remember to move your legs repeatedly during the flight or car trip to avoid increasing the risk of blood clots. It is very advisable to consult your doctor long enough before long or distant travel.
Sexual relationships are allowed except in those at risk of bleeding or uterine contractions.
Finally, physiotherapy and light aerobics before, during and after pregnancy help you keep a smart and healthy body and a normal weight.
What are the dates I should see my obstetrician at?
It is best to consult a doctor as soon as possible during pregnancy to allow for early diagnosis or prevention of problems. During the first visit, you will undergo a general examination of your body, heart and cervix (neck of the womb). A pelvic ultrasonography is done to evaluate the pregnancy and routine blood + urine tests are requested to screen for common problems.
Then, the normal healthy lady would come to see her doctor once monthly to follow her bodyweight, fetal growth and blood pressure. Another ultrasonography is needed at 12 and 20 weeks to look for any anomalies. Monthly visits are continued till 32 weeks (8 months), then twice monthly and finally weekly visits during the last 4 weeks.
What are the routine tests requested during pregnancy?
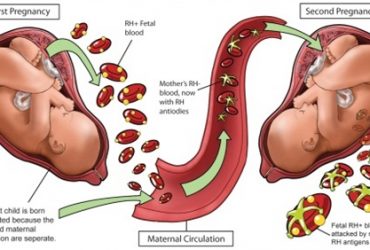
On your first few visits, the doctor usually orders screening tests for problems which are common during pregnancy, such as blood hemoglobin and blood group, liver functions, immunity to rubella and toxoplasmosis. A urine test is advisable to screen for urine or kidney diseases.
Then, your general health follow up would involve serially checking your body weight, blood pressure and urine analysis. Blood screening for diabetes mellitus (high blood sugar) is usually done at 24 & 32 weeks unless you have high risk of developing Diabetes (here you may be screened in your first few visits).
Finally, antenatal care may discover some problems or diseases may be discovered on routine screening or when the lady reports any complaints.

What are the abnormal symptoms to be reported to the doctor?
Of course, the first and most important is bleeding of whatever amount at any point in pregnancy. Second, comes cramping lower tummy pain which may feel similar to period pains. The symptoms which should also be reported as soon as possible include fever and a gush of large amounts of clear fluid per vagina (Rupture of membranes) or cough, lower limb or face edema, pain on passing urine, continuous headache, or chronic skin itching. Finally, observing the fetal kicks is important especially during the last trimester of pregnancy.
And how does the doctor decide the date and mode of delivery?
The safest way of delivery (unless otherwise indicated) is the spontaneous onset of labor pains and vaginal delivery. It is best to wait for spontaneous labor as long as the woman passes her due date.
In some cases, otherwise, the doctor may advise induction of labor using different medicines or may advise elective cesarean delivery, as in cases of hypertension, diabetes mellitus, bleeding, fetal distress or malpresentations such as breech presentation.
What is the duration of a normal labor and how may I reduce labor pains?
It is highly advisable to discuss the details of the plan for delivery in advance. This allows the lady to understand all what will happen on the day of delivery, which reduces any associated stress. The duration of labor varies between cases and may be difficult to predict until the labor starts. Yet, there so many ways to reduce labor pains to easily tolerated levels. For instance, the lady is advised to choose a good companion during labor, who may be a friend or a relative. It is also best if she visits her place of delivery in advance to reduce the feeling of unease. It is also a good idea to spend some time selecting the clothes and the room which make her comfortable.
It was proven that allowing mobility and listening to music or friendly chats help reduce labor pains and alleviates stress which helps the labor to progress efficiently. Also, the pain killing medicines in labor which may be used safely are numerous, including tablets, injections, infusions, inhalers or epidural infusions. The latter is the most effective pain-relieving choice, it is currently available in most labor wards, but it needs an experienced anesthetist to determine whether there are any problems which may contraindicate its use.
What are most important postnatal advises?
The lady should start walking as soon as possible after delivery. She should pay attention to personal hygiene and cleanliness of hands and breasts. She should report any problems such as excessive bleeding, fever, chest pain, leg swelling, or breast discomfort.

As for the neonate, breast feeding is the best staring as early as possible. A normal neonate does not need any additional nutrition other than breastmilk which (although being of little amount in the first 1-2 days after delivery) is usually concentrated and rich in nutritive. Adding water or boiled drinks may cause diarrhea or distension to the baby and may make him/her refuse breast milk later on.
During the first week after delivery, it is normal for babies to lose 10% of their weight. It is also normal to develop mild jaundice, especially between the 3rd-7th day.
But it is advisable to consult the doctor urgently in case of neonatal continuous screaming even after feeding, severe jaundice especially during the first 2 days, poor breast feeding, fever, constipation or diarrhea.
The newborn needs eye drops to prevent infections after delivery. It also needs to have the umbilical scar sterilized repeatedly during the first few days. The baby should also not be overdressed in to much clothing to avoid excessive sweating and dehydration/fever. Since neonates have some progressive bleeding tendency during the first few weeks, it is advisable to give a vitamin K injection and to avoid surgery (such as circumcision) beyond the first 24 hours after delivery until 6 weeks postnatally to avoid excessive bleeding.
The neonatologist should be consulted during the first few weeks to follow up the neonate’s health. Some tests are done routinely since very young age, such as thyroid hormone testing. Some vaccines should also be given as early as possible such as hepatitis B and tuberculosis to protect the newborn.
Best Regards
Dr. Sherif Ahmed Ashoush