My blood group is Rh-negative, is this a dangerous condition?
There are no or minimal risks as long as you take the necessary precautions. As you may know, blood groups may be A, B, AB or O. Any of these types may be positive or negative from the point of view Rh typing. A blood group is a hereditary state which forms in utero according to the blood group of the parents. Thus, the baby may have a different blood group than the mother.
What are the risks associated with different blood groups in the mother and her baby?
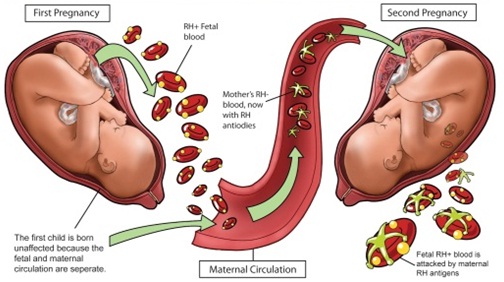
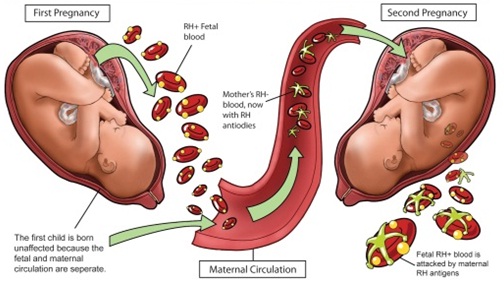
The mother with an Rh-Negative blood group may form an immune reaction against the baby’s Rh-positive blood group. This may lead to hemolysis (destruction of the baby’s red blood cells) presenting as severe anemia and jaundice after delivery.
Since the maternal and fetal blood do not mix unless following bleeding during pregnancy or at delivery, the first pregnancy passes smoothly in most cases and problems start presenting during the following pregnancies.
What are the complications of developing an immune reaction against the baby’s blood group?
These complications occur only if the blood group of the following baby is also Rh-positive. Here, the mother’s body starts forming large amounts of antibodies against the baby’s red blood cells leading to their destruction.
The results of such destruction depend on the severity of the immune reaction. Mild cases may develop some mild anemia after delivery.
Moderate cases develop postnatal jaundice, usually requiring treatment (phototherapy) and admission to a Special Care Baby Unit to prevent this condition from harming the baby’s brain. While in severe cases, the baby develops severe anemia during pregnancy, leading to its heart failure and possible death.

Should this happen to all women with an Rh-negative blood group?
It only happens to those carrying a baby with an Rh-positive blood group, inherited from the father. Subsequently, an Rh-negative woman is only at risk if her husband’s blood group is Rh-positive. Even in such cases, only 20-25% of cases develop a reaction to the baby’s Rh blood group.
How may I prevent such complications?
If your Rh blood group is negative while your husband’s group is positive, then you must have an Anti-D injection. This contains antibodies which stop your body forming an immune reaction. This injection is effective only in those who did not develop any immune reaction yet (= only as a preventive measure, not useful in those who already developed immune reaction).
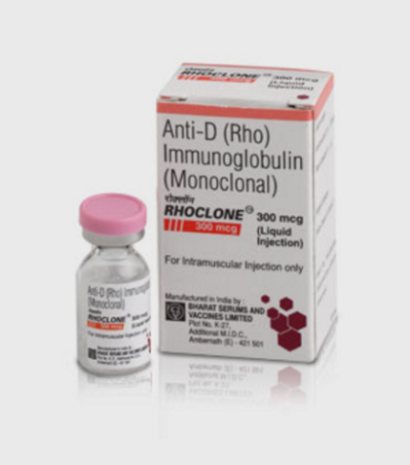
The Anti-D (Rh) injection should be administered during the first 3 days (best within the first day after delivery, bleeding or miscarriage). It should be repeated after every pregnancy or in case of bleeding or intrauterine intervention during pregnancy. Recent research proved that an additional injection at 28 and 32 weeks of pregnancy further reduces the risks of maternal sensitization and hence developing any complications from 2% to 0.2%.
Should I repeat these injections with every pregnancy?
Yes, unless your newborn is Rh negative, like your Rh type. Unfortunately, this may only be diagnosed at delivery, thus it is still advisable to receive the Anti-D injections during pregnancy, then to test the newborn’s blood group at birth to identify the need for another injection at delivery.

What if the bleeding is recurrent during the same pregnancy, should I receive an injection with each new attack?
An injection gives you enough protection for about 6 weeks following moderate bleeding. So, you do not need any additional injection unless the new attack of bleeding is severe or happens >6weeks after the last Anti-D injection.
What about if I have already developed a reaction to Rh-positive blood groups, or if I already developed complications in my pregnancy due to Rh immunization?
Then the Anti-D injection is of no use. Your pregnancy needs strict follow up with an experienced doctor. The baby requires follow up scans to identify the severity of the disease. Some babies need premature delivery, intrauterine blood transfusion, post-natal admission to intensive care units and/or phototherapy.
Are there any risks associated with different A-B-O groups or other types of blood groups?
This is rare & usually is mild enough to present only after birth with no high risks to your baby.
Wishing you the best of health