The importance of controlling the blood glucose during pregnancy:
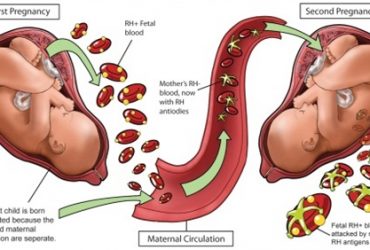
Uncontrolled blood glucose during pregnancy may lead to complications to you and/or your baby, the vast majority of which may be prevented by strict control of diabetes mellitus starting few months before any planned pregnancy. These complications include maternal hypertension, eye diseases, poor immunity and increased risks of complications during labor. Fetal complications include large size, anomalies, in utero distress or needing neonatal intensive care admission.

How may I control my blood sugar during pregnancy?
This needs strict control of your diet, exercise plans and medications. Insulin injections are the safest option during pregnancy since it can not cause any fetal anomalies.
Since your blood glucose may change throughout the day, depending on your food intake and amount of physical exercise, your dose of insulin needs to be controlled according to frequent blood testing with every meal. This dose may also be reduced with strict food intake containing stable amounts of calories, together with light physical exercise.

A pregnancy should not be allowed to happen except after controlling your blood glucose level over the preceding 3 months, which may be checked using blood testing for HbA1c.
Some mild cases may use oral Metformin tablets, especially in the type of diabetes which presents for the first time in the second half of pregnancy (Gestational Diabetes Mellitus) or with mild cases of late onset (type II) diabetes mellitus, as long as your blood glucose is monitored strictly and supplementary low doses of insulin injections are used when required.
Testing for blood glucose to adjust the dose of insulin:
This is easiest and least painful using the home test devices which are easy to find in pharmacies. But you should serially calibrate these devices to make sure their results stay reliable.

The required (ideal) blood glucose level at each meal is as follows:
| Before Dinner | Before Lunch | Before light Brunch | None | Before Breakfast | Meal |
| 10-11 PM | 5-6 PM | 1-2 PM | 9-10 AM | 7-8 AM | Time |
| < 105 | < 105 | < 105 | < 120 | 70-90 | Glucose level (mg/dl) |
| * A slightly higher blood glucose (by 10-15 mg/dl) may be occasionally acceptable at starting treatment or according to doctors’ advice. | |||||
The main dose of insulin
Insulin is usually given in two doses, one at 7-8 am and another at 5-6 pm. The main dose is decided by the doctor, according to the lady’s bodyweight, then is further fine-tuned according to personal response.
Each dose is given as a subcutaneously, best using human insulin types, in two separate injections: intermediate acting (type N) and short acting (type R). The latter’s dose may be occasionally changed according to the specific glucose level at the time of injection. Occasionally, another injection may be added in case of high blood glucose at the noon or dinner time.

How to decide on the amount of additional insulin with any of the previous meals?
We usually add one unit of Insulin (type R) for every increase in blood glucose of 10 mg/dl higher than the ideal blood glucose level at the specific meal. For example, if the blood glucose result prior to your 5 PM meal is 150 mg/dl, you need 4 additional units of insulin (type R) on top of your usual dose, for this day only (refer to the aforementioned table).
The advisable amount of food and caloric intake
The total daily caloric intake should be limited to 25 Kcal/Kg (calculated based on pre-pregnancy bodyweight). In severe cases, this may be further reduced to 20 Kcal/Kg. Generally, very tight caloric restriction to reduce body weight is not advisable during pregnancy, unlike to non-pregnant diabetics.
This caloric intake should then be divided in small, frequent meals at fixed times in the day, making sure that most of your food intake is in the form of vegetables and fibres, a third is in the form of proteins (such as meat, fish, chicken or beans), and 10% of fats.

Schedule of usual and supplementary insulin doses
| At Dinner
(10-11 PM) |
At Lunch
(5-6 PM) |
At light Brunch
(1-2 PM) |
After Breakfast (9-10 AM) | At Breakfast
(7-8 AM) |
Meal |
| Nothing | N+R | Nothing | Nothing | N+R | Fixed usual dose |
| Nothing or
Extra R according to test result |
Nothing or
Extra R according to test result |
Nothing or
Extra R according to test result |
Nothing | Nothing or
Extra R according to test result |
Additional dose |
Instructions related to insulin intake.
- Inulin type N & R should be given in separate injections and never mixed together.
- Insulin should always be stored in the refrigerator.
- Insulin should be given at fixed times in the day.
- Use the adequate insulin syringes, i.e. 40 units syringes for the 40 units ampoules, and 100 units syringes for 100 units ampoules.
- Insulin should be injected subcutaneously, not intramuscularly or intravenously, in different injection sites each time.
- Always eat your meal at the time as insulin injections. Eating should never be postponed after insulin injections to avoid excessive lowering of blood glucose.

Diabetes Mellitus is a chronic disease, but its symptoms ad complications may be avoided considerably with strict control, commitment and regular follow-up.
Treatment is not only using medicines: control of body weight, dietary intake, and physical exercise are of utmost importance.
Early diagnosis and frequent follow up visits to an experienced specialist are important, especially during pregnancy.
To avoid fetal malformations, it is crucial to avoid pregnancy until blood glucose level is controlled for 3 months prior to pregnancy.
Wishing you the best of health