My last pregnancy ended by miscarriage, what may be the cause?
First, I must clarify that most miscarriages, especially those occurring during the first 10 weeks of pregnancy, will not happen again except rarely. Most of them are due to some random genetic abnormality which happened by chance in one of the huge number of eggs and sperms produced in the human body. And because most of the genetically abnormal embryos actually miscarry instead of carry on and ending in a malformed liveborn baby, thus giving chanced for a well-formed normal baby to replace this malformed one.

Recurrent miscarriage is a different condition, where miscarriage is repeated more than 2-3 times, indicating investigation and treatment.
What are the causes of Recurrent Miscarriage?
The reason may be a congenital defect in the womb cavity, or a weakness in the neck of the womb (uterine cervix), or adhesions in the uterine cavity.
The reason may also be a chronic infection in the uterine cervix leading to inducing contractions or preterm premature rupture of membranes (breaking the waters). It also may be due to rare genetic problems in one of the parents which is transmitted to all of the embryos conceived.
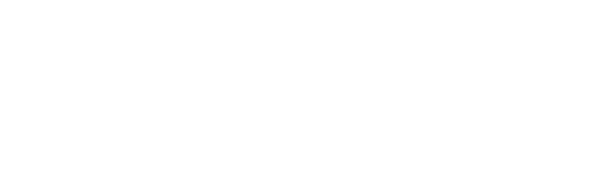
Other reasons include maternal diseases such as diabetes mellitus or autoimmune diseases such as systemic lupus erythematosis, or it may be due to some diseases in the immune balance during pregnancy, leading to the immunity attacking the embryos, or different conditions leading to excessive blood clotting, reducing the blood flow through the placenta to the embryo.
How are such conditions diagnosed?
An experienced specialist should be consulted, since some of these conditions are difficult to diagnose and some need special laboratory tests which need a long experience in the field to be properly interpreted. Occasionally, a specialist in genetics may also be consulted by the treating obstetrician/gynecologist.
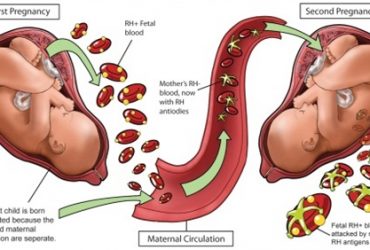
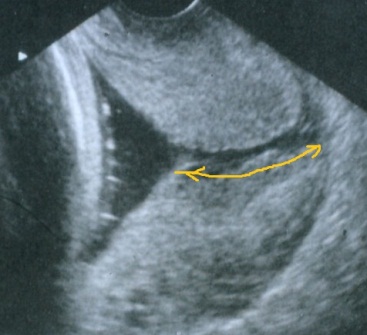
Diagnosis also needs a general clinical assessment, a pelvic ultrasonography, some blood tests or a hysteroscopy or dye test to check the uterine cavity. Some cases still remain undiagnosed, but many of them actually have a good prognosis in following pregnancies.
What about infections such as toxoplamosis or some viral infections?
Actually, this is a public misconception. Such diseases are dangerous if they begin during a pregnancy, they also cause only one miscarriage and are not causes for recurrent miscarriages. Thus, there is no point in treating them for the sake of preventing recurrent miscarriage.
What are the types of treatment?
This really needs to be individualized and tailored depending on the reason behind pregnancy loss in each case. For example, a weak cervix may benefit from progesterone medications and/or a cervical stitch. Some uterine congenital anomalies or intrauterine adhesions may need hysteroscopic treatment under anesthetics. Cases of immune defects and/or blood clotting diseases need anticoagulants, corticosteroids and/or intralipid infusions. Lastly, some genetic diseases may benefit from preimplantation genetic testing as part of an IVF cycle with the aim of looking for normal embryos to transfer into the womb.
What are the chances of success in such cases?
It depends on the mother’s age, the cause of miscarriage and the treating doctor’s experience. For instance, immune problems, being a commoncause of recurrent miscarriage, need a well experienced doctor who knows enough about such conditions, their investigations and treatment choices. Only then, such conditions may actually develop a success rate approaching 90%. Same with cases due to weakness of the womb’s neck (cervical insufficiency), these may do very well as long as they are closely monitored throughout pregnancy. Cases due to intrauterine adhesions have poorer prognosis and need an experienced surgeon to divide them.
Finally, I would like to confirm that, in presence of no apparent cause, the chances of a future pregnancy to end successfully approach 65%.

Best Regards
Dr. Sherif Ahmed Ashoush